July 29, 2025
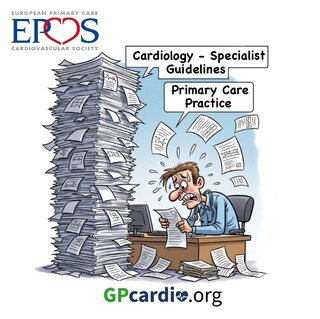
CVD & Primary Care: The need for EPCCS Practice Guidance
The EPCCS board and council members have recently convened to address critical needs supporting primary care professionals in managing the increasing burden of cardiovascular disease. As one of our primary initiatives, we are launching Practice Guidance based on the latest specialist guidelines.
The gap between cardiology specialist guidelines and their implementation in practice by primary care physicians (PCPs) is a significant challenge in healthcare, impacting patient outcomes and contributing to the burden of cardiovascular diseases (CVD). This discrepancy stems from a variety of factors, leading to suboptimal prevention and management of cardiovascular conditions in primary care settings
Considered key aspects of this gap are:
1. Underestimation of Cardiovascular Risk
- Physician-Perceived vs. Calculated Risk: Studies consistently show a significant discrepancy between how PCPs perceive a patient's cardiovascular risk and the risk calculated using validated tools like SCORE2/SCORE2-OP. PCPs often underestimate true CV risk, leading to inadequate preventive measures.
- Impact on Treatment: This underestimation directly translates to lower rates of achieving LDL-C targets and reduced use of guideline-recommended therapies, such as statins, even in high-risk patients.
2. Complexity and Volume of Guidelines:
- Information Overload: Cardiology guidelines, especially from organizations like the European Society of Cardiology (ESC), American Heart Association (AHA) and American College of Cardiology (ACC), are comprehensive and frequently updated, offering a vast array of recommendations. This can be overwhelming for PCPs who manage a broad spectrum of conditions.
- Difficulty in Application: The sheer volume and detail can make it challenging for PCPs to integrate all recommendations into their daily practice, particularly when balancing multiple patient needs and time constraints.
3. Barriers to Implementation in Primary Care:
- Time Constraints: PCPs often have limited time during patient visits, making in-depth discussions about complex cardiovascular risk and lifestyle modifications difficult.
- Resource Limitations: Insufficient resources, including staffing, diagnostic tools, and access to specialized services, can hinder adherence to guidelines, especially in lower-income settings.
- Diagnostic Complexity: Some cardiovascular conditions or risk assessments can be diagnostically complex, requiring tools and expertise that may not always be readily available in primary care.
- Lack of Training and Education: While PCPs are knowledgeable, they may not always have specialized training in the nuances of the latest cardiology guidelines or the skills needed for effective patient counseling on lifestyle changes.
- Perceived Lack of Applicability: PCPs might feel that certain guidelines, often designed by specialists for more complex cases, do not fully apply to their general patient population or may lead to "overdiagnosis and overtreatment."
- Patient Factors: Patient non-adherence to medication, lifestyle recommendations, and follow-up appointments also contributes to the gap. This can be due to a misunderstanding of their condition, cultural practices, economic factors, or a lack of adequate support.
- Therapeutic Inertia: This refers to the failure of healthcare providers to initiate or intensify therapy when indicated by clinical guidelines, even when patients are not at target. This is particularly noted in lipid management.
- Discordance Among Healthcare Professionals: Sometimes, there can be a lack of cohesive messaging or collaboration between cardiologists and PCPs, leading to inconsistencies in patient management.
4. Impact of the Gap:
- Suboptimal Patient Outcomes: The direct consequence is that many patients do not receive optimal evidence-based care for cardiovascular disease prevention and management, leading to preventable morbidity and mortality.
- Increased Healthcare Burden: Suboptimal management can lead to more severe disease progression, increased hospitalizations, and higher healthcare costs in the long run.
- Health Inequalities: Discrepancies in guideline implementation can exacerbate existing health inequalities, with vulnerable populations often being particularly undertreated.
Strategies to Bridge the Gap:
- Enhanced Education and Training: Targeted educational programs for PCPs on guideline updates and practical implementation strategies.
- Simplified and User-Friendly Guidelines: Developing guidelines that are concise, clear, and specifically tailored for primary care settings, perhaps with decision-support tools.
- Integrated Care Models: Fostering better collaboration and communication between cardiologists and PCPs through shared care plans, referral pathways, and multidisciplinary team approaches.
- Technology and Decision Support: Utilizing electronic health records (EHRs) with built-in reminders, clinical decision support systems, and risk assessment calculators.
- Patient Education and Engagement: Empowering patients with a better understanding of their risk and the importance of adherence through educational materials, counseling, and shared decision-making.
- Addressing Systemic Barriers: Advocating for policies that provide adequate time for patient encounters, appropriate reimbursement for preventive services, and improved access to resources.
- Behavioral Economics Principles: Applying principles that influence behavior to improve patient and provider adherence.
- Pharmacist and Nurse-Led Interventions: Involving pharmacists and nurses in medication management and patient counseling can significantly improve adherence.
Bridging this gap requires a multifaceted approach that addresses the systemic, professional, and patient-level barriers to guideline adherence, ultimately aiming to ensure that all patients receive the highest quality of cardiovascular care
References